
PHYSICAL INACTIVITY, DID YOU KNOW?
Physical inactivity has become a global health issue.
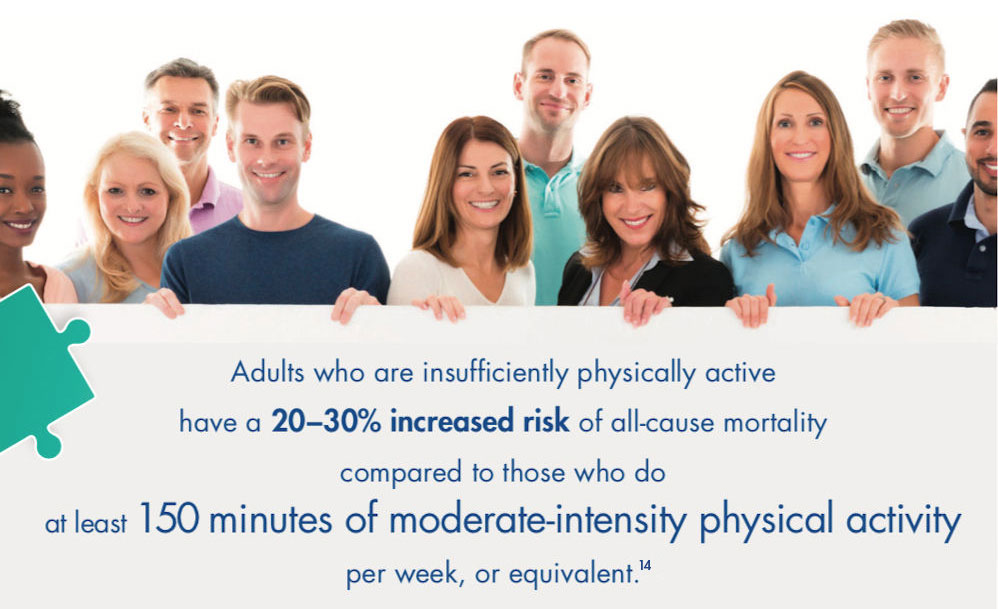
¼ adults around the world is insufficiently active.1*
Physical inactivity has been identified as the 4th leading risk factor for global mortality, with responsibility for 6% deaths worldwide.2
It is also recognized as an important risk factor for multiple chronic diseases and conditions such as Chronic Venous Disease9.
*23%, it doesn’t include inactive people.
REFERENCES
1.https://www.who.int/news-room/fact-sheets/detail/physical-activity
2.https://www.who.int/dietphysicalactivity/pa/en/
9. Lohr JM, Bush RL. Venous disease in women: epidemiology, manifestations, and treatment. J Vasc Surg. 2013 Apr;57(4 Suppl):37S-45S.
-

Physical inactivity and Risk Factors
-

Physical Activity
-

Physical activity guidelines
What is Physical Inactivity?
Physical inactivity is defined as an insufficient level of moderate to vigorous intensity of physical activity regarding the physical activity guidelines.3
Not to be confused with sedentary behavior, which has its own negative effects on health, and is defined as any waking behavior characterized by a very low energy expenditure (≤ 1.5 kcal/kg/hour), while in a sitting, reclining, or lying posture.4
What are the risk factors?
Strong scientific evidence exists for physical inactivity as a primary and actual cause or risk factor for most major chronic diseases, including:
- Hypertension and stroke
- Type 2 diabetes(5)
- Obesity and overweight(5)
- Bone health and osteoporosis(6,7)
- Cancer, particularly breast and colon cancers(6)
- Brain health and conditions that affect cognition such as depression and anxiety, and Alzheimer’s disease6,8
- All major cardiovascular diseases, i.e. diseases that affect heart and blood vessels9
Although less known, some lifestyle and occupational activities are also well-identified risk factors for venous diseases.9
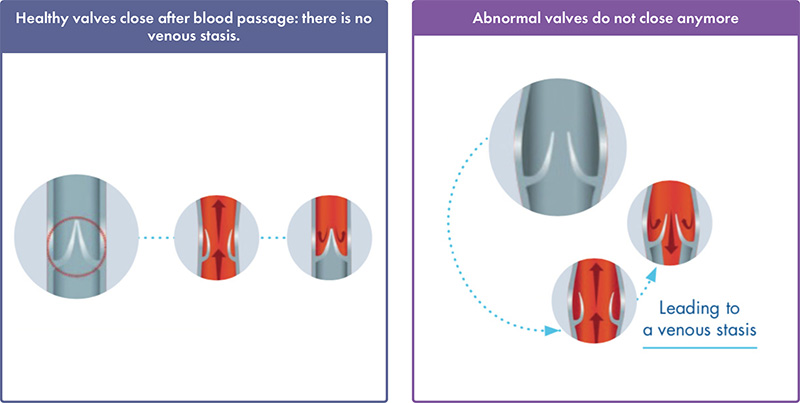
Indeed, venous reflux, i.e. the stasis of blood in legs, that causes venous insufficiency symptoms is clearly associated with lack of physical activity and absence of regular exercice.9,10
REFERENCES
3. ANSES Opinion, 2012.
4. Tremblay et al. Sedentary behavior Research Network (SBRN) – Terminology Consensus Project process and outcome. International Journal of Behavioral Nutrition and Physical Activity. 2017; 14:75.
5. WHO. Global recommendations on physical activity for health. World Health Organization. ISBN 978 92 4 159 997 9.
6. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012; 2(2): 1143 – 1211.
7. Carter MI, Hinton PS. Physical activity and bone health. Mo Med. 2014 Jan-Feb;111(1):59-64.
8. Booth FW, Roberts CK, Thyfault JP, Ruegsegger GN, Toedebusch RG. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol Rev. 2017 Oct 1;97(4):1351-1402.
9. Lohr JM, Bush RL. Venous disease in women: epidemiology, manifestations, and treatment. J Vasc Surg. 2013 Apr;57(4 Suppl):37S-45S.
10. Vuylsteke, M. E., S. Thomis, G. Guillaume, M. L. Modliszewski, N. Weides, and I. Staelens.‘Epidemiological Study on Chronic Venous Disease in Belgium and Luxembourg: Prevalence, Risk Factors, and Symptomatology’. European Journal of Vascular and Endovascular Surgery: The Official Journal of the European Society for Vascular Surgery 49, no. 4 (April 2015): 432–39.
14. https://www.who.int/gho/ncd/risk_factors/physical_ activity_text/en/
What is Physical Activity?
Physical activity is defined as any bodily movement produced by the contraction of skeletal muscle that increases energy expenditure above resting metabolic rate.12
MODERATE-INTENSITY13
Moderate-intensity physical activities take some effort, but you can still speak easily while doing these activities.
![]()
Brisk walking, recreational swimming, household tasks, riding a bike, gardening.
VIGORОUS-INTENSITY13
Vigorous-intensity physical activities require more effort, making you breathe harder and faster.
![]()
Aerobics, running team sports or hard manual labor, fast cycling or swimming.
MUSCLE-STRENGTHENING13
Muscle-strengthening activities cause the body’s muscles to work or hold against an applied force or weight.
![]()
Yoga, lifting heavy objects multiple times to strengthen various muscle groups, working with resistance bands.
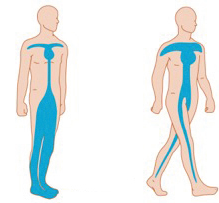
How walking decreases venous stasis?
Walking, even a few steps, significantly improves venous flux and symptoms in healthy individuals. The venous pump function can also be reactivated by activities such as biking, swimming or aquagym.11
Preferably, aerobic activity should be performed in bouts of 10 minutes or more and spread throughout the week.
REFERENCES
11. Glauser F, Codreanu A, Tribout B, Mazzolai L, Depairon M. Prévention de la maladie veineuse chronique : quels conseils donner à nos patients? Rev Med Suisse. 2012;8: 306-10.
12. Thivel D, Tremblay A, Genin PM, Panahi S, Rivièere D, Duclos M. Physical activity, inactivity,and sedentary behaviors: definitions and implications in occupational health. Front Public Health. 2018;6: 288.
13. https://www.who.int/dietphysicalactivity/physical_activity_ intensity/en/
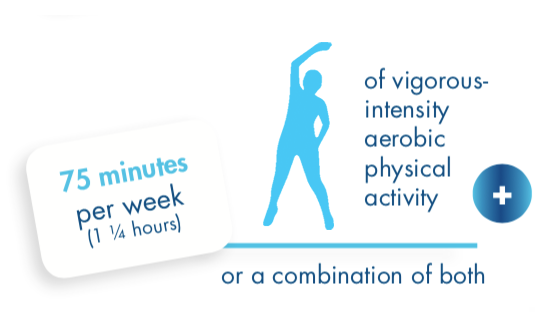
Physical Activity guidelines
Describe the amount and types of physical activity that offer substantial health benefits.
The WHO (World Health Organization) recommends that each adult aged 18-64 should accumulate at least.5


Practical Advices
Physical activity needs to be a regular and permanent habit. There are multiple ways of accumulating the total of 150 minutes per week of moderate-intensity physical activity.
MOVE MORE…
- Do what you can, some physical activity is better than none.
- Integrate physical activity as part of your every day life: spread it throughout the week.
- Start slowly if you have been inactive for a long time and increase gradually the amounts.
- Speak with your doctor or health professional if you're unsure about your health or how active to be.
- Wear appropriate clothing and footwear, eat well and drink enough water.
… SIT LESS!
- Plan your physical activity. Make a regular time for it in your diary.
- Set some realistic and reachable goals and break into smaller ones.
- Track your progress using step-counting devices (e.g. podometer) or any other apps (e.g. Map my walk/hike/ride under Armour) to motivate yourself.
Physical activity practical advices
Along your route

- For short trips, walk or cycle and leave the car at home.
- For longer trips, walk or cycle part of the way.
- Use the stairs instead of the lift.
- Get off the bus one stop earlier and walk the rest of the way.
At work

- Walk instead of emailing or making a phone call.
- Leave your desk at lunch time and enjoy a short walk outside.
- Organize walking or standing meetings.
- Take a break to move or to stretch at your desk.
Active and fun

- Catch up with friends for a walk, instead of sitting to chat.
- Plan outdoor activities, like bike riding or walking.
- Try indoor activities like dancing, indoor swimming, squash or indoor rock climbing.
Why should we follow WHO's recommendations?
Having a regular moderate-to-vigorous physical activity as recommended by the WHO can15:
- Reduce the risk of:
- All-cause mortality by 33%;
- Cardiovascular disease;
- Type 2 diabetes and help control blood glucose;
- Developing some cancers.
- Maintain or improve blood pressure.
- Help prevent unhealthy weight gain over time.
- Slow the decline in bone density and the loss of muscles.
- Reduce the feelings of anxiety.
REFERENCES
5. WHO. Global recommendations on physical activity for health. World Health Organization. ISBN 978 92 4 159 997 9.
15. Physical Activity Guidelines for Americans, 2nd edition | 2018 U.S. Department of Health and Human Services.
Physical Inactivity: TAKE THE TEST!

CHRONIC VENOUS DISEASE, DID YOU KNOW?10
41% of the world population are in the early stages of venous disease
Around 20% of patients with no clinical signs suffer from pain, heavy legs, etc...
Around 21% of patients with telangiectasia or reticular veins irrespective of symptoms
ARE YOU SURE ABOUT YOUR VEINS HEALTH?
Pregnancy and chronic venous disease
During pregnancy, women are more at risk of developing varicose veins11 and deep vein thrombosis.12
During pregnancy, some drugs may not be appropriate to relieve from pain in the legs, but compression stockings can be used7.
REFERENCES
7. Nicolaides, Andrew N., and Nicos Labropoulos. ‘Burden and Suffering in Chronic Venous Disease’. Advances in Therapy 36, no. Suppl 1 (March 2019): 1–4.
11. Ismail, Lars, Pasha Normahani, Nigel J. Standfield, and Usman Jaffer. ‘A Systematic Review and Meta-Analysis of the Risk for Development of Varicose Veins in Women with a History of Pregnancy’. Journal of Vascular Surgery. Venous and Lymphatic Disorders 4, no. 4 (2016): 518-524.e1. https://doi.org/10.1016/j.jvsv.2016.06.003.
12. James, Andra H. ‘Venous Thromboembolism in Pregnancy’. Arteriosclerosis, Thrombosis, and Vascular Biology 29, no. 3 (March 2009): 326–31. https://doi.org/10.1161/ ATVBAHA.109.184127.
-

What is Chronic Venous Disease?
-

Risk factors
-

What are the different treatment methods?
What is Chronic Venous Disease?
Chronic Venous Disease (CVD) refers to chronic conditions related to or caused by veins that become diseased or abnormal and do not work effectively.
Valves become inefficient. It becomes difficult for blood to pass through the vein walls and to flow back to the heart.
What are the symptoms experienced by patients?
The symptoms felt by the patient are the leading cause of consultation in vascular medicine and can be experienced in the early disease.
- Feeling of heaviness in the legs
- Pain in the legs
- Feeling of swelling in the legs
- Night cramps
There may be other symptoms such as:
- Sensation of 'pins and needles' in the legs
- Sensation of burning in the legs
- Sensation of tightness in the legs
- Itching with or without visible cutaneous lesion in the legs
- Feeling of tiredness
- Restless legs
Symptoms are most commonly felt in the calves and tend to increase as:1,2,3
- The day goes on and during hot weather
- After prolonged sitting/standing position
- At the end of the day and/or during night
These symptoms might be due to other conditions than venous disease. On the other hand, the absence of symptoms doesn't exclude a venous disease.
REFERENCES
1. Benigni JP et al. Venous symptoms in C0 and C1 patients: UIP consensus document. Int Angiol. Vol. 32. N°3. 2013, p261-265.
2. Guex JJ et al. The “C0s” patient: worldwide results from the Vein Consult Program. Phlebolymphology. Vol 19. N°4. 2012, p182-192.
3. Perrin MR. Description and definition of venous symptoms in chronic venous disorders: a review. Medicographia. Vol 37, N°1. 2015, p10-15.
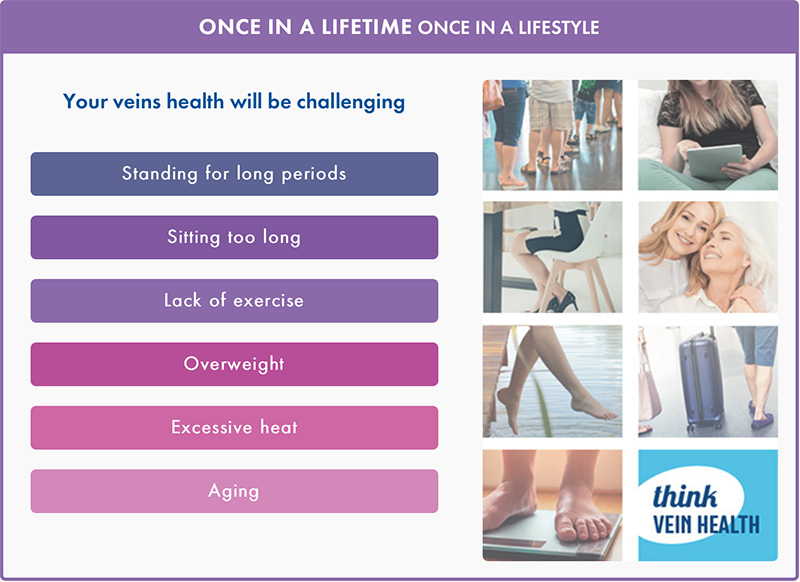
What are the main risk factors?
The main risk factors of developing Chronic Venous Disease are:4, 5, 6
- Age (veins do not contract as easily as we get older)
- Family history of chronic venous insufficiency
- Pregnancy & number of pregnancies
- Sedentary lifestyle
- Prolonged sitting/standing position
- Thromboembolic disorders
- Obesity/overweight
- High heel shoes
How is Chronic Venous Disease diagnosed?
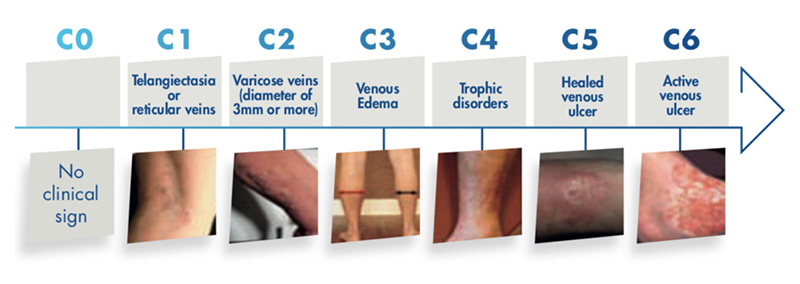
A diagnosis is made by combining the visual examination of the legs (CEAP classification) and symptoms felt by the patient.
In addition, it is necessary for the doctor to perform a Doppler or Duplex Ultrasound in order to determine if there is a reflux and/or an obstruction in veins and how severe it is.7
The CEAP classification (Clinical-Etiology-Anatomy-Pathophysiology) is used to classify chronic venous disorders, which are heterogenous among patients. The Clinical part is divided from C0 (no clinical sign) to C6 (open ulcer) according the severity of the disease.8
Examining your legs, try to know in which category you are:
What may be the ultimate complications of the disease?
Situation leading to a venous stasis are most at risk of developing a venous thrombosis, which may be of very serious concern.9
Deep vein thrombosis is the formation or presence of a thrombus in the deep veins. It occurs mostly in the lower extremities. It can cause serious injuries of the legs, including limb swelling, pain, discoloration, itching, and ulcer formation.
Even more dramatic, when the thrombus moves from deep veins of the legs until pulmonary artery or its branches, it can cause an obstruction of the artery, called a Pulmonary embolism. It is a major cause of mortality worldwide.
Prevention of Deep Venous thrombosis thereby decreases the incidence of Pulmonary Embolism.
REFERENCES
4. Tedeschi Filho, Wagner, Nei R. A. Dezzotti, Edvaldo E. Joviliano, Takachi Moriya, and Carlos Eli Piccinato. ‘Influence of High-Heeled Shoes on Venous Function in Young Women’. Journal of Vascular Surgery 56, no. 4 (October 2012): 1039–44.
5. Vuylsteke, M. E., S. Thomis, G. Guillaume, M. L. Modliszewski, N. Weides, and I. Staelens. ‘Epidemiological Study on Chronic Venous Disease in Belgium and Luxembourg: Prevalence, Risk Factors, and Symptomatology’. European Journal of Vascular and Endovascular Surgery: The Official Journal of the European Society for Vascular Surgery 49, no. 4 (April 2015): 432–39.
6. Wittens, C., A. H. Davies, N. Bækgaard, R. Broholm, A. Cavezzi, S. Chastanet, M. de Wolf, et al. ‘Editor’s Choice - Management of Chronic Venous Disease: Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS)’. European Journal of Vascular and Endovascular Surgery: The Official Journal of the European Society for Vascular Surgery 49, no. 6 (June 2015): 678–737.
7. Nicolaides, Andrew N., and Nicos Labropoulos. ‘Burden and Suffering in Chronic Venous Disease’. Advances in Therapy 36, no. Suppl 1 (March 2019): 1–4.
8. Eklöf et al. Revision of the CEAP classification for chronic venous disorders: Consensus statement. From the American Venous Forum. Journal of Vascular Surgery. Vol 40, N°6. p1248-1252.
9. Badireddy, Madhu, and Vasudeva Ranjit Mudipalli. ‘Deep Venous Thrombosis (DVT) Prophylaxis’. In StatPearls. Treasure Island (FL): StatPearls Publishing, 2019. http://www.ncbi.nlm.nih.gov/books/NBK534865/.
11. Ismail, Lars, Pasha Normahani, Nigel J. Standfield, and Usman Jaffer. ‘A Systematic Review and Meta-Analysis of the Risk for Development of Varicose Veins in Women with a History of Pregnancy’. Journal of Vascular Surgery. Venous and Lymphatic Disorders 4, no. 4 (2016): 518-524.e1. https://doi.org/10.1016/j.jvsv.2016.06.003.
12. James, Andra H. ‘Venous Thromboembolism in Pregnancy’. Arteriosclerosis, Thrombosis, and Vascular Biology 29, no. 3 (March 2009): 326–31. https://doi.org/10.1161/ ATVBAHA.109.184127.
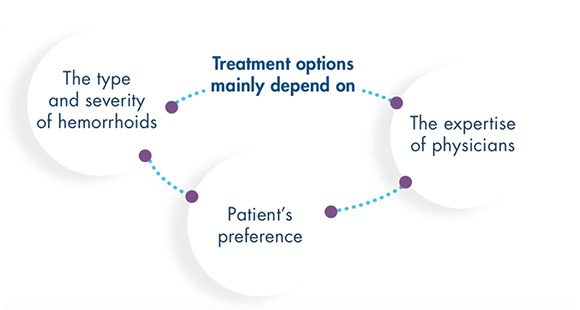
What are the different treatment methods?
The Chronic Venous Disease therapy should be either systemic, or local. In addition, venotonics and elastic compression (or compression therapy) occupies not the last place in it.
Before starting any treatment, it is essential to consult your doctor or pharmacist for advice.
PHLEBOTONIC DRUGS
Phlebotonic drugs comprise a heterogenous group of drugs, some of which are synthetic whereas most are of plant origin. Although the mode of action of these drugs is not fully understood, it seems clear that products can act at both the microcirculation and Macrocirculation levels, improving the venous tone. Most of them have shown anti-inflammatory effects, and flavonoids have also shown antioxidant properties.
Diosmin, coumarin, horse chestnut seed extract, gingko extracts, calcium dobesilate, are among the most widely prescribed products to help relieving pain, heavy legs and other functional symptoms.7
COMPRESSION STOCKINGS
Compression stockings apply pressure to the legs, reducing venous reflux and helping blood to come back to the heart. The pressure to be used depends on the stage of the disease. They decrease functional signs (pain, heavy legs etc.) and have a significant effect on the patient quality of life. They are also essential at the latest stages of the disease, in case of edema and skin damages.
Compression stocking are available in different formats and they can be used in pregnancy.
As an alternative to compression stockings, bandages can also be used.(7)
VARICOSE VEINS REMOVALS
Until recently, the traditional vein ligations with or without stripping has been the gold standard for varicose veins treatment. Although surgery provides good outcomes, it is associated with adverse effects (such as ecchymosis, hematoma, tenderness, infection, etc.).
Less invasive treatments are available:
- Sclerotherapy (sclerosing agent is introduced in the vein, inducing damages of the varicose vein, which tend to disappear after fibrosis).
- Endovenous laser ablation (EVLA) and radio-frequency ablation (RFA), and other treatments have also been developed as alternative to sclerotherapy and surgery.13
REFERENCES
7. Nicolaides, Andrew N., and Nicos Labropoulos. ‘Burden and Suffering in Chronic Venous Disease’. Advances in Therapy 36, no. Suppl 1 (March 2019): 1–4.
13. Belramman, Amjad, Roshan Bootun, Tristan R. A. Lane, and Alun H. Davies. ‘Endovenous Management of Varicose Veins’. Angiology 70, no. 5 (May 2019): 388–96. https://doi.org/10.1177/0003319718780049.
Chronic Venous Disease: TAKE THE TEST!

What are hemorrhoids?
Hemorrhoids are cushions of highly vascular tissue that are located at the anal canal of all healthy individuals.1,2
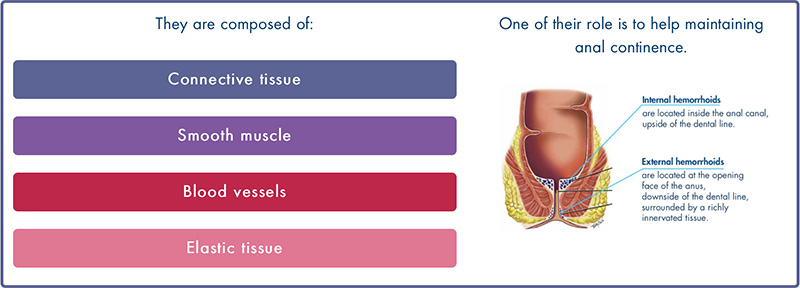
Although hemorrhoids are normal structures, the term “hemorrhoids” has come to refer to pathologic condition more scientifically called hemorrhoidal disease or sometimes hemorrhoidal crisis.
REFERENCES
1. Sneider E.B, et al. Diagnosis and Management of Symptomatic Hemorrhoids. Surg Clin N Am 90 (2010) 17–32.
2. Sandler R.S, et al. Rethinking what we know about hemorrhoids. Clinical Gastroenterology and Hepatology 2019;17:8–15.
-

What is hemorrhoidal disease?
-

Risk factors
-

What are the treatment methods?
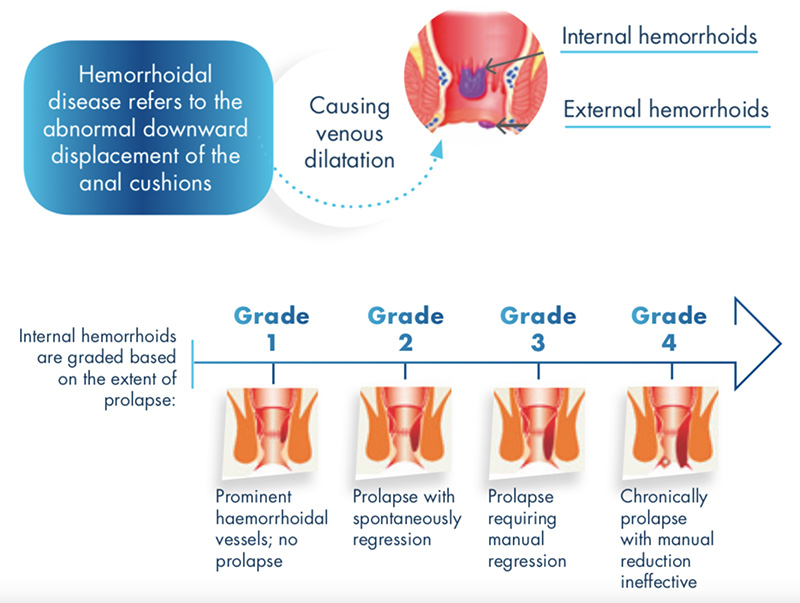
What is hemorrhoidal Disease?(3,4)
The mechanism of hemorrhoidal disease development is still poorly understood.
While in the past pathologic hemorrhoids were thought to be anorectal varices, the actual hypothesis of their origin is local tissular deterioration.
What are the manifestations of hemorrhoidal disease?(3,4)
External hemorrhoids can thrombose (formation of a blood clot in hemorrhoidal vessels) and induce:
- Acute and throbbing pain (Most common symptom).
- Sensation of a painful perianal mass.
- Dark and clotted bleeding.
Internal hemorrhoids can prolapse and/or thrombose, inducing:
- Red bleeding (most common symptom, it usually happens during defecation and it is almost always painless. Blood coats the stools and is found on toilet paper and/or into the bowl).
- Moderate fecal incontinence.
- Irritation of perianal skin (Itching or burning).
- Mucus discharge.
- Pain (more rarely).
- Sensation of tissue prolapse or perianal fullness.
Under normal circumstances
- Hemorrhoidal disease is generally painless with only local discomfort feeling.
- An hemorrhoidal crisis refers to an exacerbation of symptoms (i.g. an acute and throbbing pain that occurs in conjunction.

REFERENCES
3. Sun. Z et al. Review of Hemorrhoid Disease: Presentation and Management. Clin Colon Rectal Surg (2016). 29, 22–29.
4. Geçim E., et al. Haemorrhoidal Disease Management. EMJ Gastroenterol. 2017; 6[Suppl 6]:2-12.
What are the risk factors of hemorrhoidal disease?3,4,5,6,7
Identified risk factors of hemorrhoidal disease include
- Overweight
- Prolonged defecating position / sitting position
- Situations in which abdominal pressure is increased
- Insufficient dietary fibers intake
- Heavy lifting
- Transit dysregulation - constipation, chronic diarrhea
- Family history
- Pregnancy
- Ageing
- Local impairment - Anal intercourse, rectal pathology
- Straining for defecation
- Insufficient oral fluids intake
- Alcohol, fatty or spicy food
As prolonged physical inactivity can promote constipation, it might also be considered as a risk factor of hemorrhoidal disease.
Diagnosis
Exact data on hemorrhoidal disease prevalence are rare. The true prevalence is inevitably underestimated due to the under-reporting of these symptoms. It is estimated to be up to 40% of the general population.
Are "hemorrhoids" frequent?8,9,10
Hemorrhoids are very common during pregnancy and post-partum.
Up to 85% of pregnant women
This can be explained by the physiological changes occurring during pregnancy as well as the frequent occurrence of constipation.
11% to 38% of pregnant women suffer from constipation
How should I know if I have hemorrhoidal disease?1,3
All symptoms of hemorrhoids are non-specific. Many other conditions may be concomitantly present or cause similar symptoms (anal fissure, malignancy, inflammatory bowel diseases...).
Therefore, a thorough medical examination is necessary for diagnosis. It includes:
- External inspection
- Digital examination
- Further examinations
If you experience blood in the stool, it is recommended to see a doctor as soon as possible as this sign may be caused not only by hemorrhoids but also by more severe pathologies.
REFERENCES
1. Sneider E.B, et al. Diagnosis and Management of Symptomatic Hemorrhoids. Surg Clin N Am 90 (2010) 17–32.
3. Sun. Z et al. Review of Hemorrhoid Disease: Presentation and Management. Clin Colon Rectal Surg (2016). 29, 22–29.
4. Geçim E., et al. Haemorrhoidal Disease Management. EMJ Gastroenterol. 2017; 6[Suppl 6]:2-12.
5. Margetis N. Pathophysiology of internal hemorrhoids. Annals of Gastroenterology (2019)32, 1-9.
6. Lohsiriwat V. Hemorrhoids: From basic pathophysiology to clinical management. World J Gastroenterol 2012 May 7; 18(17): 2009-2017.
7. Iovino P et al. New onset of constipation during long-term physical inactivity: a proof-of-concept study on the immobility-induced bowel changes. PLoS One. 2013 Aug 20;8(8):e72608.
8. Perera N, et al. Phlebotonics for haemorrhoids. Cochrane Database Syst Rev (2012). CD004322.
9. Riss S, et al. The prevalence of hemorrhoids in adults. Int J Colorectal Dis (2012) 27:215-220.
10. Vazquez J.C. Constipation, haemorrhoids, and heartburn in pregnancy. BMJ Clin Evid 2008.
What are the treatment methods for hemorroidal disease?
Treatment methods
External hemorrhoids
Usually require no specific treatment unless they become acutely thrombosed or causes patients discomfort.
Internal hemorrhoids
Can be effectively treated with lifestyle and dietary measures, medication, instrumental measures and/or surgery.
Lifestyle and dietary measures
The objective is to prevent or reduce pathological development or symptoms of hemorrhoidal disease.
It includes:
- Increasing dietary fibers and oral fluids intake consumption.
- Avoiding straining and prolonged defecation position.
- Avoiding anal intercourse.
- Performing regular exercise.
Having a good transit regulation is essential!
Before starting any treatment, it is essential to consult your doctor or pharmacist for advice.
INSTRUMENTAL AND SURGICAL TREATMENT
The objective is to induce fibrotic scarring of internal hemorrhoids.
- Rubber band ligation: Hemorrhoids are tied off with rubber bands leading to their obliteration.
- Infrared coagulation: The infrared light converted into heat allows coagulation of hemorrhoids.
- Sclerotherapy: Sclerosant drugs are injected at the base of the hemorrhoid leading to an inflammatory response and shrinking of hemorrhoids.
- Surgery is generally restricted to the most severe forms of hemorrhoids. A wide range of technic are available.
PHARMACOLOGICAL TREATMENT
The objective is to relieve symptoms.
- Modifiers of intestinal transit can help regulate the consistency or frequency of stools.
- Phlebotonics are drugs that reduce capillary fragility and improve microcirculation in venous insufficiency. They are effective for overall symptom improvement of hemorrhoidal disease. They are recommended for short-term use in cases of acute manifestations of hemorrhoids (hemorrhoidal crisis), in particular bleeding and pain. Phlebotonics can usually be used during pregnancy lactation and post- partum.
- Non-steroidal anti-inflammatory drugs (NSAIDS), analgesics, and cortisone derivatives can be used in case of pain caused by thrombosed hemorrhoids. However they should be used carefully for safety reasons.
- Localized topical treatments (suppositories, creams or ointments) combining, to varying degrees, applied corticosteroids, anesthetics, lubricants, protectors and phlebotonics can also be indicated.
- For pregnant women, only certain medications can be used, with caution. Hip baths can help reduce hemorrhoidal pain.
REFERENCES
8. Perera N, et al. Phlebotonics for haemorrhoids. Cochrane Database Syst Rev (2012). CD004322.
11. Ohsiriwat V. Treatment of hemorrhoids: A coloproctologist’s view. World J Gastroenterol. 2015 Aug 21;21(31): 9245–9252.
12. Higuero T, et al. Guidelines for the treatment of hemorrhoids (short report). J Visc Surg (2016). 153, 213–218.
13. Abramowitz L. Management of hemorrhoid disease in the pregnant woman. Clinic and Biologic Gastroenterology (2008) 32, S210-S214.




