
What are nutritional deficiencies?
There are 2 types of nutrients:
| MACROnutrients |
|---|
| Proteins |
| Carbohydrates |
| Fats |
| MICROnutrients |
|---|
| Minerals: Calcium (CA), Magnesium (MG) |
| Trace elements: Zinc (ZN), Iron (FE), Copper (CU), I |
| Vitamins: Vit D, Vit C, Vit B |

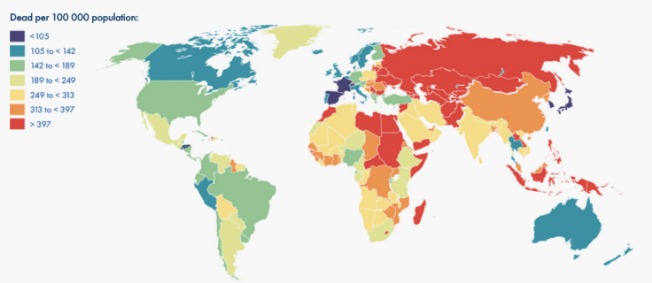
Malnutrition is the first cause of death in the world (2017)1,3
11 Millions of deaths and more than 255 millions of death disability-adjusted life years.
| Risk factors: Top 3 |
|---|
| 1. Diet high in sodium |
| 2. Diet poor in whole grains (deficiencies in Iron, Zinc, Vit B1, B2, B6, Folates) |
| 3. Diet poor in fruits (deficiencies in Vit C, Vit A, Folic acid) |

What are the causes of these nutritional deficiencies?1
Various nutritional deficiencies can have different causes:
| Decreased intakes |
|---|
| Malabsorption |
| Drug/nutrients interactions |
| Monotonous diet |
| Low intake of animal source food |
| Poverty, Poor economic status |
| Seasonal variations in food availability |
| Food shortage |
| Increased losses |
|---|
| Menstrual |
| Cycle Diarrhea |
| Parasitic infections |
| Increased needs |
|---|
| Pregnancy |
| Breastfeeding |
| Growth period |
| Acute and chronic diseases |
What are the consequences of these nutritional deficiencies?1
- Anemia
- Dental diseases
- Cognitif disorders
- Hepato-digestive disorders
- Cardiovascular diseases
- Cancers
- Neural tube defects
- Osteoporosis
- Visual disorders
- Stunted growth
- Mental retardation
- Birth defects
- Skin disorders
- Oedema
1. Lindsay A. et al. Guidelines on food fortification with micronutrients. WHO Library Cataloguing-in-Publication Data. 2006. 3-86.
2. Anuraj H Shankar. Mineral Deficiencies. Hunter’s Tropical Medicine and Emerging Infectious Disease (Ninth Edition) 2013, Pages 1003-1010
3. Afshin, A., Sur, P.J., Fay, K.A., Cornaby, L., Ferrara, G., Salama, J.S., Mullany, E.C., Abate, K.H., Abbafati, C., Abebe, Z., et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 0. (2019).
Iron deficiency and anemia
What is anemia?
Anemia is a common condition that affects 1 in 3 people worldwide.1 It is defined as a decreased number of red blood cells (RBCs) and occurs when there is an insufficient amount of iron in the body to make hemoglobin. When the quantity of hemoglobin is reduced, fewer red blood cells are formed, and the ones that are formed are smaller. Since haemoglobin is the protein that carries oxygen throughout the body, when there is not enough, the body doesn’t get all the oxygen it needs.
Certain groups are at particular risk for anemia 2, 3, 4
-

CHILDREN
-

WOMAN OF CHILDBEARING AGE
-

SURGICAL PATIENTS
-

ELDERLY
Why are children at particular risk?
Toddlers and children of preschool age have the highest prevalence of anemia at 47.4% of their population group according to the World Health Organization (WHO), largely due to nutritional choices.6
Children require more iron for growth and development, yet many children receive less than their recommended daily value. Children in this age group often receive a good supply of dairy, yet this food group is deficient in adequate iron and can ultimately increase the child’s risk of developing iron-deficiency anemia.7
What are the consequences of anemia in children?8,9,10
- LEARNING LAG
- DISTURBANCE OF COGNITIVE PERFORMANCES
- GROWTH DISTURBANCE IN CHILDREN
- DISTURBANCE OF IMMUNE STATUS
REFERENCES
6. Global anaemia prevalence and number of individuals affected. World Health Organization Web site. http://www.who.int/vmnis/anaemia/prevalence/summary/ anaemia_data_status_t2/en/. Accessed April 3, 2017.
7. Thakur N, Chandra J, Pemde H, Singh V. Anemia in severe acute malnutrition. Nutrition. 2014;30(4):440-442.
8. Bandhu R et al. Effect of iron on growth in iron deficient anemic school going children. Indian Journal of Physiology and Pharmacology. 2003. 47 (1) : 59-66.
9. Grantham-McGregor S et al. A Review of Studies on the Effect of Iron Deficiency on Cognitive Development in Children. J Nutr. 2001 Feb;131(2S-2):649S-666S.
10. Ekiz C et al. The effect of iron deficiency anemia on the function of the immune system. The Hematology Journal. 2005. 5: 579-583.
Why are women of childbearing age at particular risk?
Due to blood loss experienced through menstruation and the greater demands on the blood supply for the developing fetus during pregnancy, women tend to suffer from a high rate of anemic risk, with a global prevalence of around 42% within their population group.6
Women of childbearing age are the population with the most affected individuals, with an estimated 468 million being non-pregnant women, according to WHO5 and are the highest at-risk population group for iron-deficiency anemia.
What are the consequences of anemia in women of childbearing age?
Whilst women of child bearing age are vulnerable to iron deficiency anaemia, pregnant women in particular are at risk due to high iron requirements.
Iron deficiency anemia can, in pregnant women, lead to:11,12
- LOW BIRTH WEIGHT
- SPONTANEOUS ABORTION
- FETAL GROWTH RETARDATION
- PREMATURITY
REFERENCES
6. Global anaemia prevalence and number of individuals affected. World Health Organization Web site. http://www.who.int/vmnis/anaemia/prevalence/summary/ anaemia_data_status_t2/en/. Accessed April 3, 2017.
11. Vural T et al. Can anemia predict perinatal outcomes in different stages of pregnancy? Pakistan Journal of Medical Science. 2016. 32(6) : 1354-1359.
12. Huch R et al. Iron Deficiency and Iron Deficiency Anemia. Pocket Atlas Special. Thieme. 2006. Chapter 4 : 34-38
Why are surgical patient at particular risk?
The mean prevalence of pre-operative anemia is around 35%. The aetiology of pre-operative anemia may be multifactorial and complex. (Nutritional deficiencies, some drugs, activation of the immune system…). The mean prevalence of post-operative anemia can reach 90%. It is mainly caused by preoperative anemia and/or important blood loss during surgery.13
What are the consequences of anemia in surgical patients?
Preo-operative anemia and post operative anemia are independent risk factor for increased post-operative morbidity and mortality, as well as for prolonged length of hospital stay.13,14
REFERENCES
13. Muñoz , M., Franchini , M., and Liumbruno , G.M. (2018). The post operative management of anaemia: more efforts are needed. Blood Transfus 16, 324 325.
14. Muñoz, M., Gómez Ramírez , S., Campos, A., Ruiz, J., and Liumbruno , G.M. (2015). Pre operative anaemia: prevalence, consequences and approaches to management. Blood Transfus. Trasfus . Sangue 13, 370 379.,)
Why are the elderly at particular risk?
Anemia is common in the elderly and its prevalence increases with age.
Iron deficiency anemia, the second most common cause of anemia in the elderly, usually results from chronic gastrointestinal blood loss caused by nonsteroidal anti-inflammatory drug–induced gastritis, ulcer, colon cancer, diverticula or angiodysplasia. Older persons may also become iron deficient because of inadequate intake or inadequate absorption of iron.15
What are the consequences of anaemia in elderly patients?
Anemia in the elderly is associated with a poor prognosis that is in terms of mortality, morbidity and risk of fragility.16
REFERENCES
15. Smith DL. Anemia in the Elderly. Am Fam Physician. 2000 Oct 1;62(7):1565-1572
16. Maerevoet, M., Sattar, L., Bron, D., Gulbis, B., and Pepersack, T. (2014). [Anemia in the elderly]. Rev Med Brux 35, 361–367
How to recognize ida symptoms?5
- Chest Pain
- Shortness of breath
- Headache
- Tachycardia
- Brittle nails
- Weakness
- Mucocutaneous pallor
- Fatigue
How is anemia treated?
Anemia is often easily treated. The treatment options you receive depend on how severe the anemia is and the underlying cause.
Iron supplementation
Treatment for anemia due to iron deficiency usually involves taking iron supplements and making changes to your diet. The purpose is to treat your symptoms by increasing levels of iron and therefore haemoglobin in your body. Oral iron supplementation is available in various forms. Don’t hesitate to ask your healthcare professional about the best solution for you.
Dietary changes
Certain foods are rich in iron and should be encouraged
- Animal-source foods.
- Lean meat and seafood.
- Nuts, beans, vegetables, and forified grain products.
- Cereals and bread with extran iron in them (fortified).
- Pulses (beans, peas and lentils).
Other foods and drinks are low in iron and/or make it harder to absorb iron this large amounts should be avoided
- Black and herbal tea.
- Coffee.
- Milk and dairy.
- Foods with high levels of phytic acid - such as wholegrain cereals.
REFERENCES
1. Nicholas JK. et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014.123: 615–24.
2. Lopez A et al. Iron deficiency anaemia. Lancet. 2016 Feb 27;387(10021):907-16
3. WHO Library Cataloguing-in-Publication Data 2015. The global prevalence of anaemia in 2011.
4. Munoz M et al.‘Fit to fly’: overcoming barriers to preoperative haemoglobin optimization in surgical patients. British Journal of Anaesthesia. 2015; 115 (1): 15–24.
5. Iron Deficiency Anaemia: Assessment, Prevention and Control. A Guide For Programme Managers (Document WHO/NHD/01.3). Geneva: World Health Organization, 2001 https://www.nhlbi.nih.gov/health-topics/iron-deficiency-anemia.
Calcium & vitamin d deficiencies
Why are calcium & vitamin d important?
Vitamin D and calcium are both very important for optimal human health. Vitamin D is needed for bone mineralisation and has a major role in the absorption of calcium from the intestine, while calcium has a role in maintaining the rigidity and strength of the skeleton. Calcium is involved in a large number of metabolic processes, including blood clotting, cell adhesion, muscle contraction, hormone neurotransmitter release, glycogen metabolism, and cell proliferation and differentiation.1, 2
WHAT PROBLEMS ARE ASSOCIATED WITH CALCIUM & VITAMIN D DEFICIENCIES? WHO IS AT RISK?1,2
A lack of both vitamin D and calcium can lead to serious bone and skeletal problems. In children, this can present as rickets and in adults, as low bone mineral density and osteoporosis.1
-

YOUNG PEOPLE
-

MENOPAUSAL
-

ELDERLY
CHILDREN AND ADOLESCENTS3
Why?
Childhood and adolescence are a very important time for the formation of the skeleton. Calcium requirement is increased during this period. However, many young people do not have a proper breakfast, with its traditional variety of calcium-rich foods.
Low levels of vitamin D in children have been reported in studies worldwide, due in part to young peoples’ increasingly indoor lifestyles, pollution in urban settings, and use of sunscreen.
Which consequences?
Although rare in industrialized countries, severe vitamin D deficiency in children can lead to growth retardation and bone deformities known as rickets.
An inadequate bone health during youth result in an increased susceptibility to osteoporosis and fractures in later life.
REFERENCES
3. Bess Dawson-Hughes, Ghada El-Hajj Fuleijan & Patricia Clark. Building strong bones in children and adolescents. International Osteoporosis Fondation. World Osteoporosis Day 2013.
WOMEN GOING THROUGH OR POST MENOPAUSAL PERIOD3
Why?
Oestrogen plays a vital role in regulating the bone turnover process throughout life. However, as women become oestrogen deficient when menses cease, bone resorption exceed bone formation and is associated with a decrease in calcium intestinal absorption and calcium kidney retention.
Which consequences?
One in three women over the age of 50 will suffer a fracture caused by osteoporosis. result in an increased susceptibility to osteoporosis and fractures in later life.
REFERENCES
3. Bess Dawson-Hughes, Ghada El-Hajj Fuleijan & Patricia Clark. Building strong bones in children and adolescents. International Osteoporosis Fondation. World Osteoporosis Day 2013.
THE ELDERLY4
Why?
The elderly are often subject to malnutrition and reduced sunlight exposure.
In addition, their calcium intestinal absorption and calcium kidney retention are decreased, as well as, their capacity to synthetise vitamin D and convert it to its active form.
Which consequences?
Fractures due to osteoporosis are a major cause of pain, long-term disability and loss of independence among older adults, and can even result in premature death.
REFERENCES
4. Cyrus Cooper, Bess Dawson-Hughes, Catherine M. Gordon, René Rizzoli. Healthy Nutrition, Healthy Bones. International Osteoporosis Fondation. World Osteoporosis Day 2015.
- People on diets poor in calcium and vitamin D.
- As vitamin D is also produced by exposure to sunlight, people who do not get exposure to enough sun and do not make up through dietary vitamin D consumption are at risk.
What are the long-term risks of these deficiencies?5
What are the signs or symptoms?
- Increased risk of fractures.
- The development or worsening of skeletal disorders: Ricket, osteomalacia.
- Stunted growth.
- Osteoporosis.
There are often no clear symptoms of vitamin D and calcium deficiencies, except in more severe cases.

How are calcium & vitamin d deficiencies treated?
Responsible sun exposure
The main source of vitamin D is sunlight (UVB irradiation).
Our skin can make vitamin D from exposure to sunlight.
However sunlight is not a reliable source of vitamin D and there are also associated risks of skin ageing and cancer.5
Dietary changes
Calcium
- Milk
- Yogurt, Cheese
- Tofu, Soya bean
- Curly kale
- Sardines
- Figs, whitebait, almonds
Vitamin D
- Salmon, sardines, meckerel
- Tuna
- Cod liver oil
- Shiitake mushrooms
- Egg yolk
You may be referred to a specialist dietician if you need specific guidance about increasing the amount of vitamin D or calcium in your diet.
Supplements
If your diet does not provide adequate amounts of calcium or vitamin D, or you are allergic to certain foods it may be a good idea to add supplements to the diet.
Calcium supplements should be combined with vitamin D for optimum effect.
Ask your pharmacist or you GP about the best options available for you.
REFERENCES
1. Lindsay A. et al. Guidelines on foodfortification withmicronutrients. WHO Library Cataloguing-inPublicationData. 2006. 3-86.
2.Heike A. Bischoff-Ferrari. Threestepsto unbreakablebones, vitaminD, calcium and exercise. International OsteoporosisFondation. World OsteoporosisDay 2011.
3. Bess Dawson-Hughes, GhadaEl-Hajj Fuleijan& Patricia Clark. Bonescare for postmenopausalwomen. International OsteoporosisFondation. World OsteoporosisDay 2013.
4. Cyrus Cooper, Bess Dawson-Hughes, Catherine M. Gordon, René Rizzoli. Healthy Nutrition, Healthy Bones. International OsteoporosisFondation. World OsteoporosisDay 2015.
5. Heike A. Bischoff-Ferrari. THREE STEPS TO UNBREAKABLE BONES, VITAMIN D, CALCIUM AND EXERCISE. International OsteoporosisFondation. World OsteoporosisDay 2011.




